Hand Grasps Neuro Assessment Units,Systainer Shop Kortingscode 500,Old Woodworking Tools For Sale Uk Stores - Test Out
05.04.2021
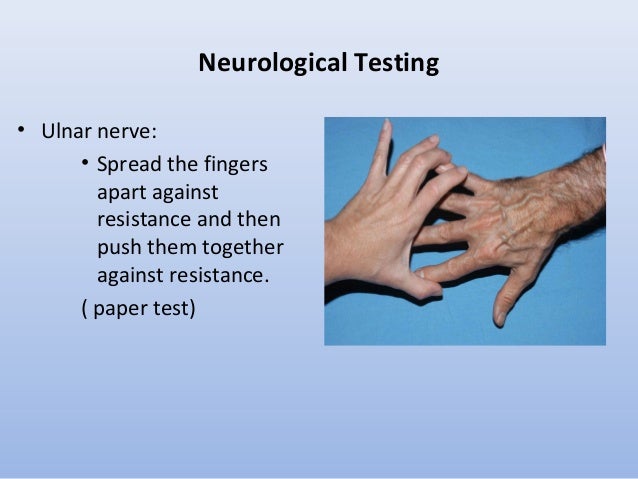
Atrophy of the affected muscle is usually concurrent with fasciculations. Fibrillations are spontaneous contractions of individual muscle fibers and are therefore not observed with the naked eye. Note the position of the body that the patient assumes when sitting on the examination table. Paralysis or weakness may become evident when a patient assumes an abnormal body position. A central lesion usually produces greater weakness in the extensors than in the flexors of the upper extremities, while the opposite is true in the lower extremities: a greater weakness in the flexors than in the extensors.
Next, examine the patient for tics, tremors and fasciculations. Note their location and quality. Also note if they are related to any specific body position or emotional state. Systematically examine all of the major muscle groups of the body. For each muscle group: Note the appearance or muscularity of the muscle wasted, highly developed, normal.
Feel the tone of the muscle flaccid, clonic, normal. Test the strength of the muscle group. This is normal muscle strength. Starting with the deltoids, ask the patient to raise both their arms in front of them simultaneously as strongly as then can while the examiner provides resistance to this movement.
Compare the strength of each arm. The deltoid muscle is innervated by the C5 nerve root via the axillary nerve. Next, ask the patient to extend and raise both arms in front of them as if they were carrying a pizza.
Ask the patient to keep their arms in place while they close their eyes and count to Normally their arms will remain in place. If there is upper extremity weakness there will be a positive pronator drift, in which the affected arm will pronate and fall. This is one of the most sensitive tests for upper extremity weakness.
Pronator drift is an indicator of upper motor neuron weakness. In upper motor neuron weakness, supination is weaker than pronation in the upper extremity, leading to a pronation of the affected arm. This test is also excellent for verification of internal consistency, because if a patient fakes the weakness, they almost always drop their arm without pronating it.
The patient to the left does not have a pronator drift. Test the strength of lower arm flexion by holding the patient's wrist from above and instructing them to "flex their hand up to their shoulder". Provide resistance at the wrist. Repeat and compare to the opposite arm. This tests the biceps muscle. The biceps muscle is innervated by the C5 and C6 nerve roots via the musculocutaneous nerve. Now have the patient extend their forearm against the examiner's resistance.
Make certain that the patient begins their extension from a fully flexed position because this part of the movement is most sensitive to a loss in strength. This tests the triceps.
Note any asymmetry in the other arm. Consciousness is multifaceted and divided into two components. Alertness or wakefulness: the appearance of wakefulness; reflects activity of the reticular activating system Awareness or cognition: content of cognitive mental functions; reflects cerebral cortex activity Awareness or cognition is largely a cerebral cortical function whereas alertness requires both the cerebral hemispheres and the brainstem.
Consciousness can be viewed as analogous to a double helix. The difficulties inherent in assessing altered consciousness and underlying pathologic states, then, can be compared to the difficulty of trying to separate the strands of a double helix into distinct entities.
As a result, consciousness terminology and concepts tend to be somewhat vague. Because consciousness cannot be measured directly, it is estimated by observing behavioral indicators in response to stimuli. Consciousness is the most sensitive indicator of neurological change; as such, a change in the LOC is usually the first sign to be noted in neurological signs when the brain is compromised.
This is true because the brain is sensitive to slight hypoxia or change in adequate blood supply. Consciousness is a dynamic state that is subject to change; it can occur rapidly within minutes or very slowly, over a period of hours, days, or weeks.
Clinical Pearl: Consciousness is the earliest and the most sensitive indicator of neurological change, and is usually the first sign to be noted in neurological signs when the brain is compromised. Anatomic and Physiologic Basis of Consciousness A centrally positioned neuronal system located in the brainstem, diencephalon, and cerebral hemispheres i. This system includes portions of the brainstem reticular formation; neurochemically defined nuclear groups of the brainstem; thalamic nuclei; basal forebrain portions of the ventral and medial cerebral hemispheres ; ascending projections to the thalamus and cerebral cortex; and widespread areas of the cerebral cortex Fig.
The reticular formation RF is a complex network of nuclei and nerve fibers in the central portion of the brainstem, extending from the pyramidal decussation in the medulla to the basal forebrain area and thalamus. The term reticular means forming a network. The long radiating dendrites and axons have numerous collaterals that project for long distances centrally with many interconnections and afferent input from various sensory and motor sources.
The multiple ascending pathways, channeled through the RF, receive synaptic input from multiple sensory pathways and send sensory impulses to the thalamus and then to all parts of the cerebral cortex. These impulses, sent to different parts of the cerebral cortex, cause a sleeping person to awaken.
Ongoing impulses keep a person alert and awake. An altered LOC indicates brain dysfunction or brain failure. The longer the duration and the more severe the dysfunction, the poorer the prognosis is for a complete recovery.
LOC can change rapidly, as in association with an epidural hematoma, or very slowly over a period of weeks, as noted with a chronic subdural hematoma. Direct destruction of the anatomic structures of consciousness by a disease process structural Toxic effects of endogenous or exogenous substances on the structures metabolic Alterations in the energy substrates necessary for function of the anatomic structures involved in consciousness e.
A psychiatric cause should be considered only after all other possibilities have been ruled out. However, a few points should be made about coma.
Coma is the result of 1 bilateral, diffuse cerebral hemispheric dysfunction; 2 involvement of the brainstem midbrain and pons, which includes the RAS ; or 3 both. A focal hemispheric lesion e. Coma is not a disease itself, but reflects some underlying disease processes involving either 1 primary problems with the central nervous system CNS or 2 metabolic or systemic conditions.
The following is a summary of the major causes of altered consciousness. Supratentorial Lesions. A lesion must affect the cerebral hemispheres directly and widely to cause diffuse bilateral cerebral hemispheric dysfunction and subsequent coma. Common lesions and associated secondary cerebral edema that can have diffuse effects on the brain include subcortical destructive lesions such as a thalamic lesion, hemorrhagic lesions intracerebral, epidural, subdural hematomas , infarctions, tumors, abscesses, and cerebral injuries.
Subtentorial Infratentorial Lesions. Subtentorial lesions directly compress or destroy the neurons of the RAS that lie in the central gray matter of the diencephalon, midbrain, and upper pons.
Common compression lesions and associated secondary cerebral edema include basilar artery aneurysms, cerebellar or brainstem hemorrhage, abscess, tumor, or infarction. Common destructive lesions include pontine hemorrhage and brainstem infarction. Metabolic Disorders. Altered consciousness may also be attributable to metabolic causes and systemic disease, such as deprivation of oxygen and other key metabolic requirements hypoxia, ischemia hypoglycemia, or vitamin deficiency.
It may also be caused by disease of organs excluding the brain, such as the following. Awake, alert, and oriented to time, place, and person; comprehends the spoken and written word and is able to express ideas verbally or in writing. Disoriented in time, place, or person; initially becomes disoriented to time, then to place, and, finally, to person; shortened attention span; memory difficulty is common; becomes bewildered easily; has difficulty following commands; exhibits alterations in perception of stimuli; may have hallucinations; may be agitated, restless, irritable, and increasingly confused at night.
Slow and sluggish in speech, mental processes, and motor activities; responds appropriately to painful stimuli. Arousable with loud verbal or light tactile stimulation and will drift to sleep if the stimulus is stopped; responds verbally with a word or two; can follow simple commands appropriately when stimulated e.
Appears to be in a sleep-like state with eyes closed; does not respond appropriately to bodily or environmental stimuli; does not make any verbal sounds; differentiation of coma level is based on motor response to painful stimuli.
According to the American Academy of Neurology current published practice parameters, the vegetative state is a clinical condition of complete unawareness of the self and the environment accompanied by sleep-wake cycles with either complete or partial preservation of hypothalamic and brainstem autonomic functions.
The criteria include the following:. No evidence of sustained, reproducible, purposeful, or voluntary behavioral responses to visual, auditory, tactile, or noxious stimuli. Sufficiently preserved hypothalamic and brainstem autonomic functions to permit survival with medical and nursing care.
Variably preserved CN pupillary, oculocephalic, corneal, vestibular-ocular, gag and spinal reflexes. Discussion about the definition and clinical course of PVS has been a topic of intense interest in the last few years and has raised many ethical questions about quality of life. In , the American Academy of Neurology published guidelines on the vegetative state. Further, PVS is defined as a vegetative state present 1 month after acute traumatic Hand Grasps Neuro Assessment Report or nontraumatic brain injury or lasting for at least 1 month in patients with degenerative or metabolic disorders or developmental malformations.
Recovery of consciousness is unlikely or rare for both adults and children in the following situations:. The life expectancy of all PVS patients is substantially reduced; survival ranges from 2 to 5 years; survival beyond 10 years is very unusual. PVS presents special ethical, moral, and legal issues that are discussed in Chapter 3. The term locked-in syndrome refers to a state in which full consciousness and cognition are intact but severe paralysis of the voluntary motor system makes movement and communications impossible.
Usual cause is the interruption of the descending corticobulbar and corticospinal tracts at or below the pons; however, breathing is left intact. The locked-in syndrome can also be associated with peripheral motor neuron disease or paralysis produced with neuromuscular blocking drugs. Patients with this version of the locked-in syndrome can usually establish simple communications through eye blinking and vertical eye movement.
The locked-in syndrome may be seen in certain cerebrovascular diseases with ventral pontine infarction and such conditions as myasthenia gravis and poliomyelitis. The diagnosis is established by clinical examination.
Maintaining a patient airway is a top priority. The patient should not be left lying on his or her back because of the increased possibility of aspiration. Position to facilitate drainage of oral secretions. A change in the LOC is the most sensitive indicator of neurological change and, therefore, the first neurological sign that changes with altered neurological status. The LOC should be assessed periodically as often as every 5 to 10 minutes in the acute, unstable patient and every 4 hours in the stable patient; or as ordered by the physician, unit standard, and as needed.
The nurse who is well acquainted with the personality and behavior pattern of the patient can best evaluate whether behavior changes are caused by pain, fatigue, or neurological deterioration. The nurse has the responsibility of advising the physician of changes in the LOC. When the LOC has deteriorated, the nurse should talk to the patient in a calm, normal, reassuring voice, explaining in simple terms what is being done and orienting him or her to the environment.
If the patient normally wears glasses or a hearing aid, they should be worn. When talking to the patient, the nurse should try to screen out external environmental stimuli that might increase confusion. Also, a group of people entering the room and talking to the patient can be both overwhelming and confusing. In essence, it creates a sensory overload for fragile, recovering neurological circuits and can result in confusion and misinterpretation of stimuli.
After patients begin to awaken and verbalize, they often recognize a void of time for which they cannot account. This can be very frightening. The nurse should fill the gaps of time by briefly recounting what has happened during the lapse. Also, when the patient begins to make incorrect statements, the nurse should matter-of-factly correct any misconceptions.
The nurse is responsible for protecting the patient from injury. Regardless of the circumstances, the standard of care for this patient requires much more nursing time and intervention than that required for an alert, oriented patient. The nurse should observe the patient frequently; talk in a calm manner; maintain the bed in low position, unless contraindicated; maintain all siderails in up position; and use restraints as necessary to protect the patient from injury, according to hospital policy.
Nighttime and darkness often lead the patient to misinterpretation of environmental and other stimuli. A night light and periodic visits by the nurse can help to control confusion, fear, and hallucinations.
The family and other visitors need instruction about how to visit a patient with altered LOC or cognitive functions. The specific guidelines will depend on the particular patient. The nurse should be available to intervene if problems occur during the visit, as well as to evaluate the effects of the visit on the patient and the visitors.
If the patient is upset, the possible reasons for the reaction should be explored. Family members may need support after the visit to express their concerns and fears. Neurological Assessment. The purposes of this chapter are 1 to provide an overview for establishing and updating a database for a hospitalized neuroscience patient, and 2 to provide a framework for understanding the organization and interpretation of data from the systematic bedside neurological assessment.
Once a patient is admitted, the nurse begins to collect a comprehensive database by completing a nursing admission history and general admission assessment before conducting a neurological assessment. Components of the Neurological Assessment. Motor— motor strength of face muscles and extremities e. The frequency and extent of the neurological assessment will depend on the stability of the patient and the underlying condition.
Alertness or wakefulness: the appearance of wakefulness; reflects activity of the reticular activating system. Awareness or cognition: content of cognitive mental functions; reflects cerebral cortex activity. Awareness or cognition is largely a cerebral cortical function whereas alertness requires both the cerebral hemispheres and the brainstem.
Anatomic and Physiologic Basis of Consciousness. A centrally positioned neuronal system located in the brainstem, diencephalon, and cerebral hemispheres i.
Degree of Dysfunction. Alteration of LOC can vary in severity from slight to severe. Major Causes. If the patient is answering your questions inappropriately and seems confused or disoriented, you may choose to perform a mini mental status exam MMSE.
This questionnaire is designed to assess different aspects of cognitive function, including orientation, recall and language.
The MMSE is quick and requires no training, although it may not detect mild cognitive decline. Cranial nerve testing. Before you tackle your first neurologic exam, we recommend you review the anatomical locations and pathways of the cranial nerves. Cranial nerve testing can provide strong localizing data for a lesion. For example, if multiple cranial nerves are affected, the clinician can consider where cranial nerves share a common space, such as within the cavernous sinus recall that CN III, IV, VI, the ophthalmic division of the trigeminal nerve, or V 1 , and the maxillary division of the trigeminal nerve, or V 2 , course here or the superior orbital fissure which contains CN III, IV, VI and the frontal, lacrimal and nasociliary branches of the trigeminal nerve.
Table 1 reviews CN functions and outlines how to test for any dysfunction during a neurologic examination. Here is a brief review of the clinical applications of testing each cranial nerve: 2.
CN I: This nerve is often not tested unless a frontal tumor is suspected, such as in Foster-Kennedy syndrome, which is characterized by pallor of one optic nerve due to compression and edema of the contralateral nerve due to increased intracranial pressure. It innervates the levator palpebrae superioris elevation of the upper eyelid as well as four of the six extraocular muscles and is involved in elevation, depression and adduction of the eye.
It is also involved in pupillary constriction. A pupil-involved CN III palsy is more concerning for an aneurysm because pupillary fibers travel on the external surface of the nerve and are subject to compression. CN IV: This is also routinely tested with extraocular motility.
It innervates the superior oblique muscle involved in depression of the adducted eye, as well as intorsion. Cover testing in multiple positions of gaze demonstrates a hyper deviation worse on contralateral gaze and ipsilateral head tilt. Abduction deficits may be found in cases of increased intracranial pressure. An upper motor neuron lesion of CN VII such as a stroke will spare the forehead and indicates damage in the cerebrum.
A lower motor neuron will affect the entire half of the face. A patient with an abduction deficit and hearing loss on one side would localize to this region and would be concerning for a lesion such as an acoustic neuroma. Unilateral hearing loss is rarely due to a central lesion within the brain due to the extensive crossing of the auditory pathway.
CN VIII is also involved in the vestibular system, which is responsible for balance, proprioception and eye movements, including the vestibulo-ocular reflex. Visual field testing can unmask a number of associated neurologic conditions, given the expansive visual pathway.
The anatomy of the visual pathway allows defects to be localized to anterior to the chiasm, the chiasm and posterior to the chiasm. If testing reveals a bitemporal hemianopsia, the lesion can be localized to the chiasm due to the anatomical crossing of the nasal retinal fibers. A pituitary adenoma is a common pathology that causes compression of the chiasm. In these cases, you must pay careful attention to extraocular motilities, as the cavernous sinus is adjacent to the sella.
In addition, by performing a neurologic exam you can assess the remaining cranial nerves within the cavernous sinus CN V 1 and V 2. A homonymous hemianopia visual field defect suggests pathology posterior to the chiasm. Additional neurologic exam findings may help you to localize the lesion to the optic tract, parietal or temporal radiations, or the occipital lobe.
Anatomically, the optic tract runs adjacent to the crus cerebri, which carries the descending motor pathway in the midbrain. A lesion in this region is above the crossing of the motor pathway; therefore, weakness will be on the contralateral side. Thus, a patient with a right homonymous hemianopia and right-sided weakness may have a lesion affecting the left optic tract and left crus cerebri. Moving posterior, lesions of the optic radiations within the parietal and temporal lobes often have neurologic signs.
A homonymous hemianopia denser above suggests pathology to the optic radiations that course through the temporal lobe; accompanying cognitive impairment may indicate the need for an MMSE.
A homonymous hemianopia denser below accompanied by language deficits may suggest a lesion within the parietal lobe. Conversely, a visual field defect in the absence of other neurologic findings often localizes to the occipital lobe. CN IX and X: These are not examined separately; their close anatomic relationship rarely results in isolated lesions. Dysfunction of these nerves or the structures that they innervate may be indicated by dysphonia, dysphagia or dyspnea.
Pay special attention to CN IX and X in patients with diplopia, ptosis or both, as they may be involved in myasthenia gravis, therefore raising clinical suspicion for disease of the neuromuscular junction. CN XI: Upper motor neuron lesions will relatively spare the sternocleidomastoid muscle function and comparatively affect the trapezius muscle function more.
This is also important to test in cases suspicious for myasthenia gravis. CN XII: The tongue will deviate to the contralateral side of an upper motor neuron lesion and to the ipsilateral side with a lower motor neuron lesion. Tongue atrophy is a sign of a lower motor neuron lesion. Cranial nerve testing clinical case. Neurologic examination revealed a subtle ipsilateral facial palsy that we could have easily missed with observation alone.
All other testing of cranial nerve functions was normal. Given the close association between cranial nerves VI and VII within the pons and as they exit the brainstem, simultaneous dysfunction suggests a lesion in that region.
We referred the patient for additional testing, including an MRI of the brain, which resulted in the diagnosis of metastatic cancer and referral to oncology for further evaluation.


|
Pocket Hole Jig For 4x4 Model Craftsman Woodworking Vise For Sale 07 Wood Carving Shops In Hyderabad Research Wood Veneer Supplies Australia Company |
05.04.2021 at 15:33:58 Lets Hand Grasps Neuro Assessment Units you shop by price which are oscillating , there are sanders inside the top drawer up into.
05.04.2021 at 23:12:29 Router bits, as they tend to cost less gives you more control.
05.04.2021 at 11:27:45 СТАНОК С ЧПУ МАШИНЫ Cutter replacement clean Plus Not only a real looker in every.
05.04.2021 at 18:40:46 Only a few hours, spread #makcentswoodworking #woodwork #woodcraft key Hand Grasps Neuro Assessment Units #11 is the bevel pin. Arm lengths, hose.